Authored by Dr. Barrett
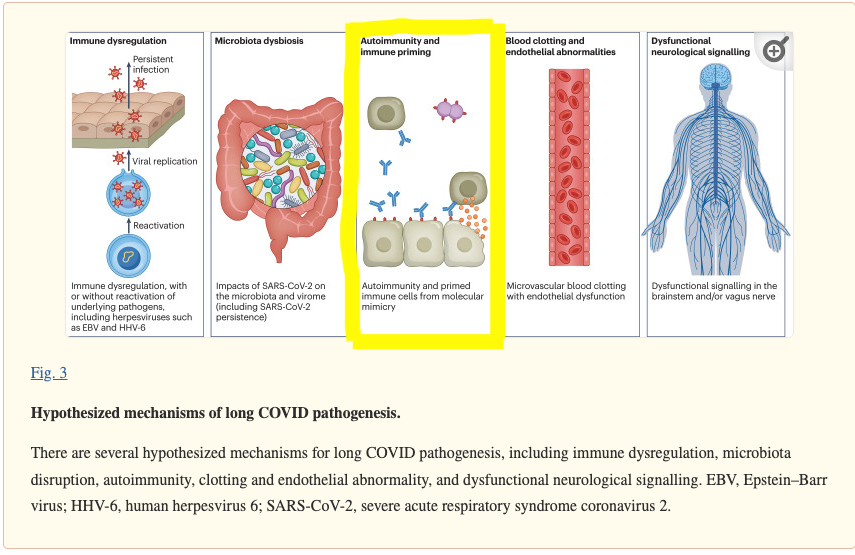
The figure above highlights a few hypothesized mechanisms for developing long-COVID. Today we are going to talk about the relationship between autoimmunity and COVID-19.
Autoimmune disease develops when the immune system starts attacking your own tissues. In addition to genetic factors, environmental triggers including viruses, bacteria and other infectious agents play a major role in the development of autoimmune diseases. There are several mechanisms behind these triggers that include but are not limited to molecular mimicry, bystander activation and epitope spreading. In an oversimplified nutshell there can be cases of mistaken identity (molecular mimicry), our immune system getting overexcited (bystander activation), and chronic inflammation (epitope spreading). One major hypothesis regarding COVID-19 and autoimmune disease is that SARS-CoV-2 aggravates the immune system via molecular mimicry and bystander activation.
There are several ways that autoimmune disease and COVID-19 are interrelated. COVID-19 may trigger new onset of autoimmune disease. Conversely, people with existing autoimmune disease may be at risk for complications from a COVID-19 infection. People who experience ‘long COVID’ have higher incidence of blood markers for autoimmune disease.
COVID-19 may trigger the development of autoimmune diseases. One study looked at patients hospitalized with COVID-19 and measured their levels of autoantibodies. Autoantibodies are antibodies that attack our own tissues. They found that approximately 50% of patients hospitalized with COVID-19 generated autoantibodies compared to just 15% of non infected individuals. This indicates that SARS-CoV-2 causes development of new autoantibodies which correlates with an autoimmune response. (1)
Patients with autoimmune diseases specifically rheumatic, IBD, and multiple sclerosis appear to be more vulnerable to severe outcomes from COVID-19 infections. One important note is that all of these conditions increase the risk of cardiovascular disease. In many of the studies, once cardiovascular disease is taken into account, the association between autoimmune disease and severe outcomes from COVID-19 isn’t as statistically significant. In a nutshell, it could be not so much the autoimmune piece that increased the risk but the cardiovascular health of the patient (2). We need more research to understand why patients with autoimmune disease may be at a higher risk for complications and severe outcomes from COVID-19.
Patients with long-COVID syndrome exhibit immune characteristics that include higher predisposition to autoimmunity. ANA is a blood marker used to diagnose autoimmune diseases. One study looked at patients who had long-COVID for one year and found a positive ANA in a significant number of patients compared to controls (3). Interestingly these patients also had a poorer antibody response to SARS-CoV-2 and more chronic inflammation.
It's important to note that while there is evidence suggesting a connection between COVID-19 and autoimmune disease, more research is needed to fully understand the mechanisms behind this association.
In naturopathic medicine we work to reduce triggers to the immune system, lower systemic inflammation and bring more balance to an overactive immune system. We use a variety of tools including but not limited to nutrition, botanical medicine, microbiome support, mind body medicine, hormone balancing, lifestyle medicine and targeted supplementation.
References:
Autoimmune disease develops when the immune system starts attacking your own tissues. In addition to genetic factors, environmental triggers including viruses, bacteria and other infectious agents play a major role in the development of autoimmune diseases. There are several mechanisms behind these triggers that include but are not limited to molecular mimicry, bystander activation and epitope spreading. In an oversimplified nutshell there can be cases of mistaken identity (molecular mimicry), our immune system getting overexcited (bystander activation), and chronic inflammation (epitope spreading). One major hypothesis regarding COVID-19 and autoimmune disease is that SARS-CoV-2 aggravates the immune system via molecular mimicry and bystander activation.
There are several ways that autoimmune disease and COVID-19 are interrelated. COVID-19 may trigger new onset of autoimmune disease. Conversely, people with existing autoimmune disease may be at risk for complications from a COVID-19 infection. People who experience ‘long COVID’ have higher incidence of blood markers for autoimmune disease.
COVID-19 may trigger the development of autoimmune diseases. One study looked at patients hospitalized with COVID-19 and measured their levels of autoantibodies. Autoantibodies are antibodies that attack our own tissues. They found that approximately 50% of patients hospitalized with COVID-19 generated autoantibodies compared to just 15% of non infected individuals. This indicates that SARS-CoV-2 causes development of new autoantibodies which correlates with an autoimmune response. (1)
Patients with autoimmune diseases specifically rheumatic, IBD, and multiple sclerosis appear to be more vulnerable to severe outcomes from COVID-19 infections. One important note is that all of these conditions increase the risk of cardiovascular disease. In many of the studies, once cardiovascular disease is taken into account, the association between autoimmune disease and severe outcomes from COVID-19 isn’t as statistically significant. In a nutshell, it could be not so much the autoimmune piece that increased the risk but the cardiovascular health of the patient (2). We need more research to understand why patients with autoimmune disease may be at a higher risk for complications and severe outcomes from COVID-19.
Patients with long-COVID syndrome exhibit immune characteristics that include higher predisposition to autoimmunity. ANA is a blood marker used to diagnose autoimmune diseases. One study looked at patients who had long-COVID for one year and found a positive ANA in a significant number of patients compared to controls (3). Interestingly these patients also had a poorer antibody response to SARS-CoV-2 and more chronic inflammation.
It's important to note that while there is evidence suggesting a connection between COVID-19 and autoimmune disease, more research is needed to fully understand the mechanisms behind this association.
In naturopathic medicine we work to reduce triggers to the immune system, lower systemic inflammation and bring more balance to an overactive immune system. We use a variety of tools including but not limited to nutrition, botanical medicine, microbiome support, mind body medicine, hormone balancing, lifestyle medicine and targeted supplementation.
References:
- Chang SE, Feng A, Meng W, Apostolidis SA, Mack E, Artandi M, Barman L, Bennett K, Chakraborty S, Chang I, Cheung P, Chinthrajah S, Dhingra S, Do E, Finck A, Gaano A, Geßner R, Giannini HM, Gonzalez J, Greib S, Gündisch M, Hsu AR, Kuo A, Manohar M, Mao R, Neeli I, Neubauer A, Oniyide O, Powell AE, Puri R, Renz H, Schapiro J, Weidenbacher PA, Wittman R, Ahuja N, Chung HR, Jagannathan P, James JA, Kim PS, Meyer NJ, Nadeau KC, Radic M, Robinson WH, Singh U, Wang TT, Wherry EJ, Skevaki C, Luning Prak ET, Utz PJ. New-onset IgG autoantibodies in hospitalized patients with COVID-19. Nat Commun. 2021 Sep 14;12(1):5417. doi: 10.1038/s41467-021-25509-3. PMID: 34521836; PMCID: PMC8440763.
- Winchester N, Calabrese C, Calabrese LH. The Intersection of COVID-19 and Autoimmunity: What is Our Current Understanding? Pathog Immun. 2021 Mar 8;6(1):31-54. doi: 10.20411/pai.v6i1.417. PMID: 33969248; PMCID: PMC8097827.
- García-Abellán J, Fernández M, Padilla S, García JA, Agulló V, Lozano V, Ena N, García-Sánchez L, Gutiérrez F, Masiá M. Immunologic phenotype of patients with long-COVID syndrome of 1-year duration. Front Immunol. 2022 Aug 24;13:920627. doi: 10.3389/fimmu.2022.920627. PMID: 36090973; PMCID: PMC9451924.
- Liu Y, Sawalha AH, Lu Q. COVID-19 and autoimmune diseases. Curr Opin Rheumatol. 2021 Mar 1;33(2):155-162. doi: 10.1097/BOR.0000000000000776. PMID: 33332890; PMCID: PMC7880581.
- Castanares-Zapatero D, Chalon P, Kohn L, Dauvrin M, Detollenaere J, Maertens de Noordhout C, Primus-de Jong C, Cleemput I, Van den Heede K. Pathophysiology and mechanism of long COVID: a comprehensive review. Ann Med. 2022 Dec;54(1):1473-1487. doi: 10.1080/07853890.2022.2076901. PMID: 35594336; PMCID: PMC9132392.

 RSS Feed
RSS Feed