Hormonal contraception such as birth control pills, hormonal IUDs (Mirena, Skyla, Kyleena, Liletta), implants, or the shot contain synthetic forms of progesterone and/or estrogen. Some types or brands of birth control will contain only synthetic progesterone while some will contain both synthetic progesterone and estrogen. Due to the route of administration and variations of hormones these types of hormonal contraception can each work a little differently, but the basics are similar. These synthetic versions of sex hormones do not act in the body the same way natural hormones do and because the body is receiving a synthetic form of these hormones it does not receive the signal to create it’s own estrogen and progesterone. Meaning hormonal contraception completely shuts down these entire hormonal pathways.
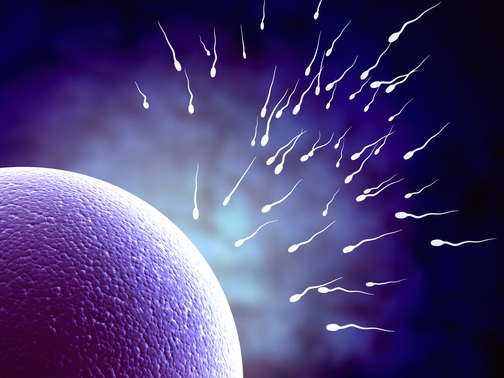
One of the most crucial ways hormonal contraception works is that it impedes ovulation from occurring. In a normal physiological state in relation to ovulation, the brain secretes hormones which then communicate to tell the ovaries to make estrogen and progesterone allowing people of reproductive age to ovulate and become pregnant if desired. When on birth control this entire communication between the brain and ovaries is non-existent. The body “thinks” it has natural estrogen and progesterone based on the synthetic hormones that are being consumed. This communication disruption does not allow ovulation to occur because the ovaries are now not receiving the signal to produce the hormones needed to develop and release a follicle.
This lack of ovulation means that the bleed that occurs on oral birth control is not technically a menses. For a monthly bleed to be considered a menses there needs to be a flux of natural hormones and ovulation must have occurred. The bleed on oral birth control instead happens due to the withdrawal of synthetic hormones while taking the placebo/sugar pills.
This lack of natural estrogen and progesterone also prevents pregnancy in many other ways besides inhibiting ovulation.
Birth control also prevents pregnancy by making cervical fluid inhospitable to sperm. Cervical fluid is necessary to become pregnant. Fertile cervical fluid which looks watery or similar to egg-white occurs immediately before ovulation. It creates a safe haven for sperm to wait until ovulation occurs, creates a sperm ‘highway’ to help the sperm travel quicker and farther into the uterus, has nutrients to feed the sperm, protects and harbors them against the more acidic vaginal pH, and filters abnormal sperm out. Normally, estrogen would signal to the cervix to make this cervical fluid, but because hormonal contraception does not allow the natural influence of estrogen to occur cervical fluid becomes thicker and less functional therefore preventing pregnancy.
While on birth control the endometrial/uterine lining of the uterus also becomes thinner. This is due to the minimal influence of natural estrogen and progesterone. As an analogy, estrogen will normally act as the bricks and progesterone acts as the mortar of the uterine lining thickening the lining throughout the course of the menstrual cycle. Without these natural influences the uterine lining is much thinner and this makes it very difficult for an embryo to implant and develop there.
IUDs can prevent pregnancy in the previous ways mentioned, but in addition can create local inflammation in the uterus as well. This prevents pregnancy by making the uterus an inhospitable place for sperm and for fertilized eggs to implant.
Hormonal contraception can also prevent pregnancy by lowering libido for some users, although this is not true for all.
All of these reasons are why hormonal contraception is so effective! It works in multiple ways to prevent pregnancy. Most forms of hormonal contraception are above 99% effective with perfect use!
Yet, for some this high level of effectiveness does not come without side effects.
Hormonal contraception has been shown to decrease libido by lowering testosterone as previously mentioned. It also can decrease the size of the clitoris. It has been studied to decrease vitamins and minerals possibly contributing to mood changes. One study even revealed that 51% of women experienced a negative mood altering effect from hormonal contraception. It has been shown to cause a slight increase in breast, cervical, and liver cancer as well. The International Agency for Research on Caner (IARC) classifies combined oral contraceptives as a group one (I) carcinogen. It can also negatively affect gut health and thyroid function. While taking oral birth control a protein called sex hormone-binding globulin (SHBG) increases in the body. It is normally responsible for binding to sex hormones in the blood and renders sex hormones inactive while attached. If this SHBG is too high it can keep too large of an amount of sex hormones inactive which can cause significant hormonal dysfunction. SHBG can stay elevated for years after discontinuation.
Also, another important side effect or result not often discussed is how hormonal contraception can be used as a ‘fix’ for issues like painful periods, endometriosis, fibroids, PCOS, or similar. But, often these conditions are not properly addressed and root causes are not treated before hormonal contraception is initiated. The first time some of these issues are addressed are when patients discontinue birth control and desire to become pregnant. I often see that because these hormonal imbalances had been masked for so long it can take a lot of time and effort to resolve, and this can be difficult when patients want to become pregnant right away. So, while hormonal birth control is a wonderful effective and widely accessible tool to help people plan their futures by preventing pregnancy, which is by far the biggest and best benefit, it absolutely does not cure hormonal issues. Hormonal contraception can actually hide hormonal issues, and the process that may be leading to these imbalances will likely go unaddressed for years until hormonal birth control is discontinued.
To learn more about what contraception choices are best for you and your life I recommend going to www.bedside.org/birth-control.com to explore hormonal and non-hormonal options.
References
1. “The Fifth Vital Sign” by Lisa Hendrickson-Jack
2. Bedsider.org








 RSS Feed
RSS Feed