This part three in a series covering autoimmune disease. Don’t miss upcoming articles covering chronic infections, environmental medicine and mind body medicine. Check out previous articles covering GI health, nutrition part 1 and nutrition part 2.
Hormone balance can often be an overlooked part of autoimmunity. I see a lot of emphasis on GI health (rightfully so) but autoimmune diseases are complex so it makes sense that the etiology is also complex.
A hormone is a signaling molecule released into circulation to target distant organs and regular physiology or behavior. In layman’s terms hormones are tiny middle managers running around the body bossing organs and tissues around. Hormones are involved in most of the activities of our bodies including digestion, sleep, stress, growth, reproduction and mood - just to name a few. We have somewhere upwards of 50 different hormones in the body with varying degrees of relationship to autoimmune disease. I am going to pick a few to highlight for you.
Estrogen
Autoimmune disease in general tends to target people with ovaries.* A current hypothesis is that estrogen might actually enhance the inflammatory process of the immune system (1). Interestingly, even the joint fluid in RA patients contains higher levels of estrogen regardless of sex (2). I will cover this more extensively in the upcoming article on autoimmune disease and environmental medicine but I want to note that we are exposed to many chemicals that are ‘estrogen-like’ (xenoestrogens) such as BPA. So it’s important to test your individual hormones as well as look at what endocrine disrupting chemicals you are exposed to in your environment.
Prolactin
Prolactin’s major role in the body is to stimulate lactation and suppress reproduction. Prolactin also stimulates the immune system as well as enhances the production of immunoglobulins and autoantibodies (3). Elevated levels of prolactin have been noted in Lupus (SLE), Rheumatoid arthritis (RA), Sjogren’s, Hashimoto’s and Multiple Sclerosis (MS) (4). Prolactin levels tend to be higher in folks with ovaries. Prolactin also elevates during chronic stress (5). Prolactin is an inexpensive blood test.
Testosterone
Testosterone levels are naturally higher in folks with testes, which might have a protective effect against autoimmune disease. The effects of estrogens on immunity have been extensively studied but less is known currently about how androgens such as testosterone impact the immune system. We do know that mice with autoimmune disease have an increase in disease activity when they are castrated (ouch!) and androgen treatment improves survival in mice with Lupus (6).
It’s important to look at the pathways. If you have a patient with low testosterone and elevated estrogen they might be converting their testosterone into estrogen via aromatase. So reducing aromatase activity is a better treatment plan than just replacing testosterone.
Cortisol
I will cover cortisol extensively in an upcoming article on mind-body medicine and autoimmune disease. In a nutshell, cortisol is supposed to be released in short bursts when we are under acute stress (running from a bear for example). Our bodies were not designed to be bathed in cortisol which is all too common these days. We have pesky chronic infections lurking behind the scenes just waiting for our immune system to be suppressed. Epstein-Barr Virus (EBV), varicella and herpes all contain stretches of DNA that sense cortisol levels and when these levels are elevated, the viruses reactivate (7). These viruses are implicated in autoimmune disease, especially EBV (8).
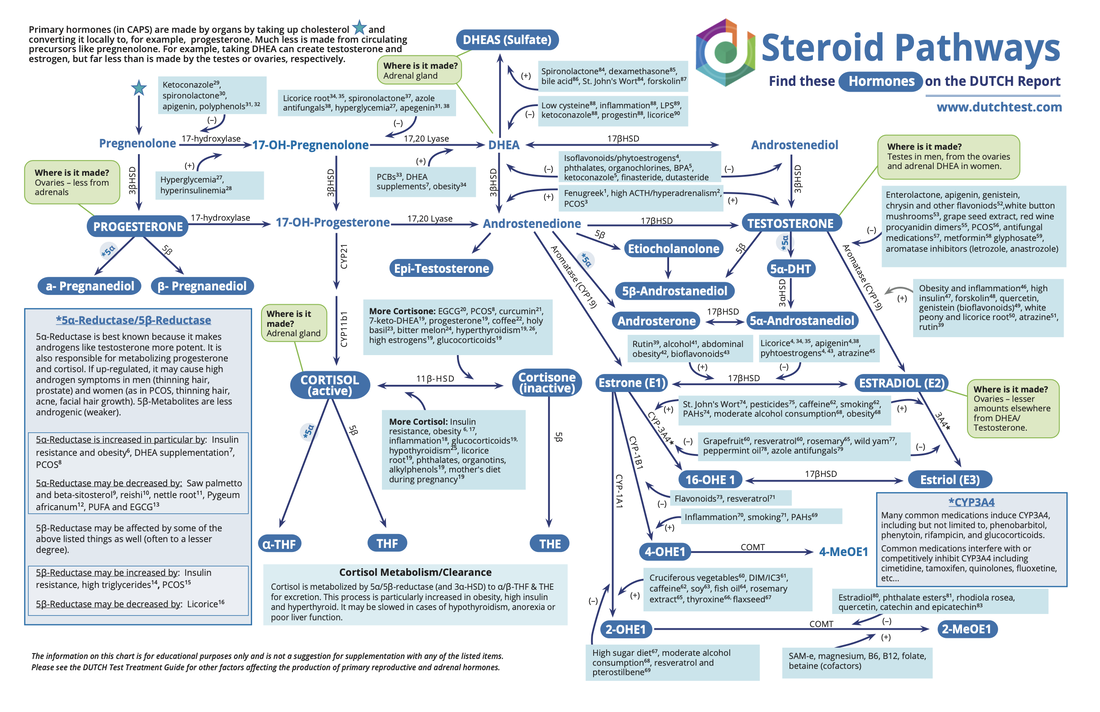
I like to use a combination of blood, saliva and dried urine (DUTCH) hormone testing to get an overall picture of hormone balance. Hormone pathways are complicated as you can see by this chart below. Just looking at a blood estrogen level isn’t enough. You can have a ‘normal’ estrogen level but if you are converting most of your estrogen into 16-OH that can make autoimmune disease worse. Testing is key.
A hormone is a signaling molecule released into circulation to target distant organs and regular physiology or behavior. In layman’s terms hormones are tiny middle managers running around the body bossing organs and tissues around. Hormones are involved in most of the activities of our bodies including digestion, sleep, stress, growth, reproduction and mood - just to name a few. We have somewhere upwards of 50 different hormones in the body with varying degrees of relationship to autoimmune disease. I am going to pick a few to highlight for you.
Estrogen
Autoimmune disease in general tends to target people with ovaries.* A current hypothesis is that estrogen might actually enhance the inflammatory process of the immune system (1). Interestingly, even the joint fluid in RA patients contains higher levels of estrogen regardless of sex (2). I will cover this more extensively in the upcoming article on autoimmune disease and environmental medicine but I want to note that we are exposed to many chemicals that are ‘estrogen-like’ (xenoestrogens) such as BPA. So it’s important to test your individual hormones as well as look at what endocrine disrupting chemicals you are exposed to in your environment.
Prolactin
Prolactin’s major role in the body is to stimulate lactation and suppress reproduction. Prolactin also stimulates the immune system as well as enhances the production of immunoglobulins and autoantibodies (3). Elevated levels of prolactin have been noted in Lupus (SLE), Rheumatoid arthritis (RA), Sjogren’s, Hashimoto’s and Multiple Sclerosis (MS) (4). Prolactin levels tend to be higher in folks with ovaries. Prolactin also elevates during chronic stress (5). Prolactin is an inexpensive blood test.
Testosterone
Testosterone levels are naturally higher in folks with testes, which might have a protective effect against autoimmune disease. The effects of estrogens on immunity have been extensively studied but less is known currently about how androgens such as testosterone impact the immune system. We do know that mice with autoimmune disease have an increase in disease activity when they are castrated (ouch!) and androgen treatment improves survival in mice with Lupus (6).
It’s important to look at the pathways. If you have a patient with low testosterone and elevated estrogen they might be converting their testosterone into estrogen via aromatase. So reducing aromatase activity is a better treatment plan than just replacing testosterone.
Cortisol
I will cover cortisol extensively in an upcoming article on mind-body medicine and autoimmune disease. In a nutshell, cortisol is supposed to be released in short bursts when we are under acute stress (running from a bear for example). Our bodies were not designed to be bathed in cortisol which is all too common these days. We have pesky chronic infections lurking behind the scenes just waiting for our immune system to be suppressed. Epstein-Barr Virus (EBV), varicella and herpes all contain stretches of DNA that sense cortisol levels and when these levels are elevated, the viruses reactivate (7). These viruses are implicated in autoimmune disease, especially EBV (8).
I like to use a combination of blood, saliva and dried urine (DUTCH) hormone testing to get an overall picture of hormone balance. Hormone pathways are complicated as you can see by this chart below. Just looking at a blood estrogen level isn’t enough. You can have a ‘normal’ estrogen level but if you are converting most of your estrogen into 16-OH that can make autoimmune disease worse. Testing is key.
If you are struggling with an autoimmune disease I recommend working with a naturopathic doctor to help identify the root cause and support your body.
*In general I do my best to use gender neutral language in my articles and presentations. We are all unique and using ‘women’ and ‘men’ just isn’t descriptive enough. Trans-men may still have ovaries, cis-women can have their ovaries removed for all sorts of reasons, etc. So I use the language ‘folks with ovaries’ and ‘folks with testes’ to be clear about the people I am talking about and the hormonal implications.
References:
*In general I do my best to use gender neutral language in my articles and presentations. We are all unique and using ‘women’ and ‘men’ just isn’t descriptive enough. Trans-men may still have ovaries, cis-women can have their ovaries removed for all sorts of reasons, etc. So I use the language ‘folks with ovaries’ and ‘folks with testes’ to be clear about the people I am talking about and the hormonal implications.
References:
- Cutolo et al. Estrogens and autoimmune disease
- Cutolo, et al. Synovial fluid estrogens in rheumatoid arthritis
- Orbach, H and Shoenfeld Y. Hyperprolactinemia and autoimmune diseases
- Shelley, S, Boaz, M and Orbach, H. Prolactin and autoimmunity
- Freeman, ME et al. Prolactin: structure, function and regulation of secretion
- Sakiana, S, Olsen, N and Kovacs, W. Gonadal steroids and humoral immunity
- Padgett, et al. Social stress and the reactivation of latent herpes simplex virus type 1
- Draborg, AH, Duus K, Houen G. Epstein-Barr Virus in Systemic Autoimmune Diseases



 RSS Feed
RSS Feed