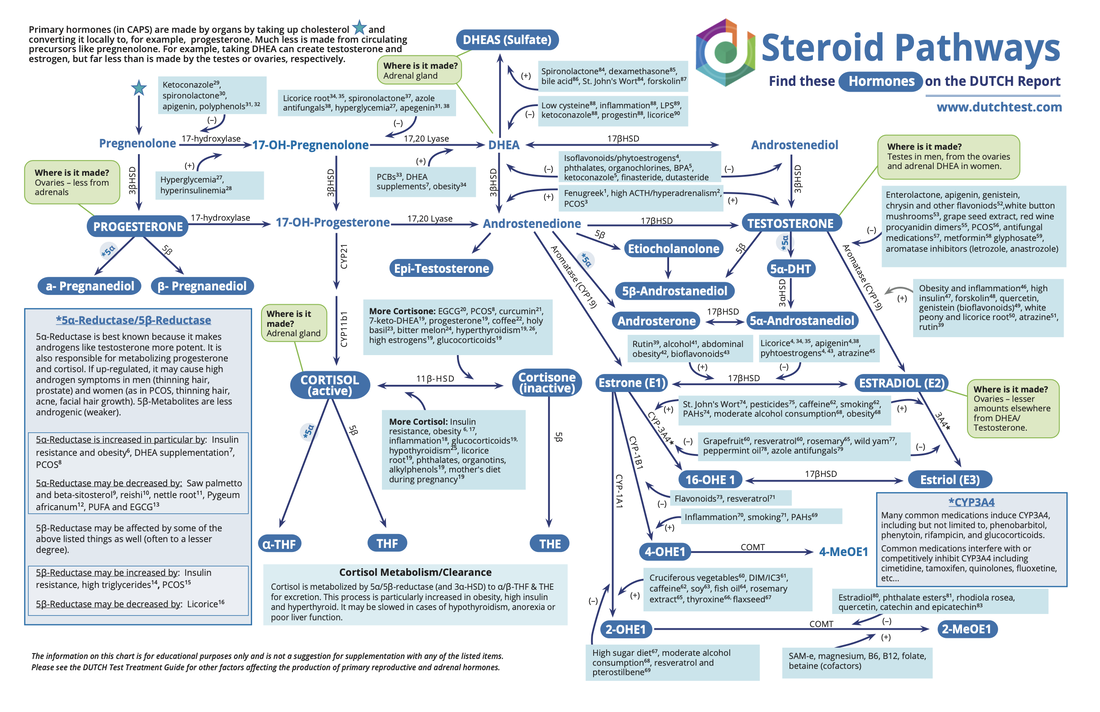
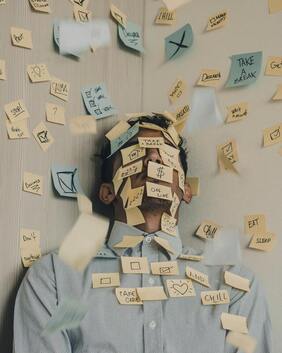
The balance between our hypothalamus, pituitary and adrenals (HPA axis) is tightly linked to our health and well being. Many of us live in a hypervigilant state with a chronically activated sympathetic nervous system. An overactive stress response can lead to elevated cortisol, insulin, inflammation, and even autoimmune disease. It’s a complicated connection and it continues to show up in my clinical practice. Just talking about "stress" with patients isn’t enough and it’s not getting to the core issues that throw our body out of balance. In my never-ending desire to understand autoimmune disease I continue to read and learn more about psychoneuroimmunology, the relationship between immunity, the endocrine system, and the central and peripheral nervous systems. A few months ago I came across the concept of "overfunctioning" and it highlights a phenomena I recognize in patients (and myself!) but didn’t have language for. As I read more about overfunctioning I realized it’s a fast track to burnout. Overfunctioning is doing more than is necessary, appropriate and healthy in our lives and relationships. This article in Psychology Today provides a laundry list of behaviors that may indicate a pattern of overfunctioning. I picked a few to share with you:
- Worrying about other people’s responsibilities.
- Taking over a group project that is coming together slowly.
- Trying to convince someone that your thinking is right.
- Furiously completing tasks for others when you feel bored, anxious, or distressed.
- Updating your friends and family about people they could contact themselves.
- Reminding your spouse or partner to call their family.
- Taking on a task at work because teaching another staff member will be frustrating.
- Doing something for your child that they can do, so it will create less of a mess.
- Giving advice to a distressed friend who hasn’t asked for any.
Dr. Sara Gotfried explains overfunctioning as:
- Doing things for others that they can do for themselves
- Absorbing other people’s feelings
- People-pleasing to avoid disappointing others
- Difficulty saying no and setting boundaries
- Assuming more responsibility than is your share
- Giving advice whether the person asks for it or not
- Fretting about others
- Feeling responsible for others, or knowing what is best for them
- Talking more than listening
- Having goals for others that they don’t have for themselves
- Codependence, or imbalanced relationships, whereby you enable someone else’s immaturity or irresponsibility through caretaking or fixing
- Behaving like a martyr, taking care of everyone else, giving without receiving, and then occasionally feeling like you were taken advantage of
- Overworking and over-scheduling yourself
There can be several core beliefs and coping mechanisms underlying overfunctioning. This article does a really excellent job of summarizing some of the roots of overfunctioning behavior. I also encourage you to work with a therapist if you resonate deeply with this information. This is challenging work. I am a recovering perfectionist and it’s easy for me to fall back into the false belief that if I want something done right, I need to do it myself. This leads me to constantly "do." I often remind myself that I am a human "being" and it’s ok to just "be" sometimes (thanks Tara Brach!)
The following are some ways you can support yourself:
- Give yourself permission to rest
- Practice saying "no." If that’s a big step for you, consider starting with "let me think about it" and give yourself a few days to make a decision.
- Creating unstructured time in your schedule
- When you feel the urge to "do" challenge yourself to get grounded first. Take a deep breath, maybe go outside and check in with yourself about your intentions and desired outcome.
- Evaluate your definition of happiness and wellbeing. Check in with yourself and make sure this is your definition and not influenced by anyone else.








 RSS Feed
RSS Feed