 Photo by Lesly Juarez on Unsplash
Photo by Lesly Juarez on Unsplash Early on in my career I met a patient with mast cell activation disorder and chronic hives. She was so ill that she had been hospitalized a few times with her throat swelling shut. We worked on all sorts of things looking at environmental triggers, using supplements to reduce histamine, changed her diet - you know, the typical naturopathic treatments. She was a little better but nothing dramatic. I lost her to follow-up and out of the blue about 6 months later she sent me a message letting me know she had found a wonderful therapist who had changed her life. Her therapist recognized that my patient had an elevated ACE (Adverse Childhood Experience) score and they had worked extensively on her childhood trauma. Much to my patients' surprise, her very difficult-to-treat condition resolved. This was a turning point for me. I started researching psychoneuroimmunology and reading everything I could about the connection between our mind and our immune system.
I am going to take a brief pause here to address what mind-body medicine IS NOT before I go on to explain all of the fascinating research. I want to be crystal clear that mind-body medicine is not about blaming the patient. I was surprised to receive an unpleasant message over social media after sharing some research on mindset and health about how unhelpful it is to point out this connection. I was surprised because I think it is incredibly empowering to know that we may be able to use our minds to heal our bodies. In my experience no one is free from the mind-body connection. We are all impacted by our minds. Once we are aware of just how powerful the connection is we are back in the driver's seat. So remember that as you continue reading. If your physical illness is manifesting in part due to emotional wounds, trauma, early childhood experiences, your mindset, etc. this does not mean that your illness is your fault AND there might even be some tools to help you.
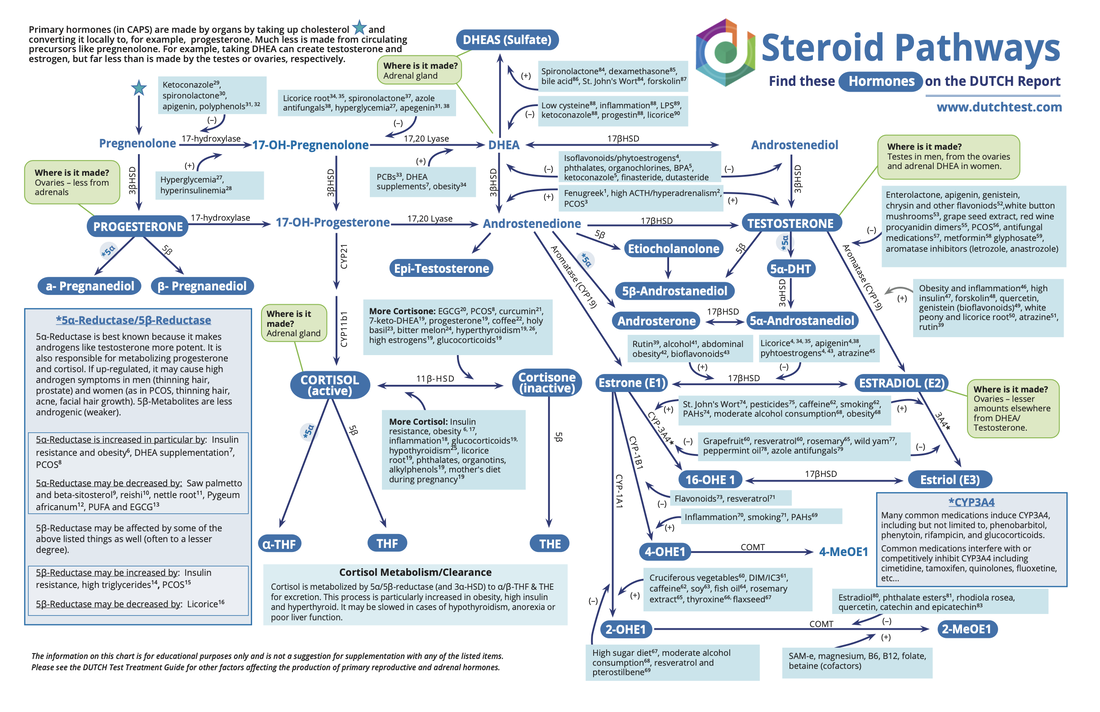
According to the Center for Mind-Body Medicine “Mind-body approaches use the conscious mind to directly affect the workings of the brain and the rest of the body. The techniques exert their effect on the hypothalamus, the switching station in the brain, which exercises control over the autonomic nervous system (which controls heart rate, blood pressure etc.), the endocrine (glandular) system and the immune system.”
The Autonomic Nervous System (ANS) is the part of the nervous system responsible for control of the bodily functions not consciously directed, such as breathing, the heartbeat, and digestive processes. It controls what is going on behind the scenes. You don’t have to think about digesting your food or sending out immune cells to fight off foreign invaders. The ANS has you covered. The ANS has two divisions, the parasympathetic and the sympathetic systems. These two systems oppose each other and ask for different responses from the organs and systems they control. For example the sympathetic nervous system will slow down digestive function while the parasympathetic system will increase digestive function.
When the sympathetic (fight, flight, or freeze) is dominant we feel more tense and alert. Stress hormones such as cortisol and epinephrine surge through our bodies. Our heart rate and blood pressure increase. Our immune cells secrete inflammatory cytokines such as IL-6 and IL-2. In contrast, when the parasympathetic (rest and digest) system is dominant we feel a sense of relaxation, tranquility and contentment. This is the baseline of balance that our body desires. Our heart rate slows, blood pressure lowers, our muscles relax and we can digest food adequately. Unfortunately, many of us are sympathetic dominant in our daily lives.
There are so many mind-body medicine topics we could cover but I am only going to pick a few since this is a blog not a book. Let’s cover self-criticism, perfectionism and loneliness. While also incredibly important, I am going to leave ACE and trauma to the experts (see the bottom for some good books to read though).
SELF-CRITICISM
When we are critical of ourselves, it has negative consequences for our health and even impacts our immune system. According to Merriam-Webster self-criticism is "the act of or capacity for criticizing one’s own faults or shortcomings." We have a complex system designed to monitor our environment for threats. When a threat is identified, we are flooded with stress hormones to help us survive. The trouble is, this system can’t differentiate between threats in our environment and threats inside our head. Criticizing ourselves activates our threat system in the same way anxiety does. Chronic stress happens when this system is constantly engaged.
Chronic stress increases interleukin-6 (IL-6). IL-6 plays an important role in signaling during an active infection. IL-6 increases inflammation and antibody production. Elevated IL-6 actually increases anxiety, alters the immune system, and increases neuro-inflammation.
We live in a culture that teaches us to be self-critical. We grow up internalizing the ideal that we must push ourselves to achieve greatness. It’s easy to put high expectations on ourselves, which leads to self-criticism when we can’t meet those expectations. Some use self-criticism as a tool to push themselves harder and harder and even fear that without the inner critic they might become "lazy."
A good rule of thumb is to stop and think about whether you would talk to someone you love the way you are talking to yourself. Most people would never speak to another person the way they speak to themselves.
PERFECTIONISM
Perfectionists are often the harshest self critics. Brené Brown, Ph.D defines perfectionism as “a self-destructive and addictive belief system that fuels this primary thought: If I look perfect and do everything perfectly, I can avoid or minimize the painful feelings of blame, judgement, and shame.”
Self-criticism is used as a way to ensure you are "perfect." The lie perfectionists tell themselves is that constant second guessing means you will not make a mistake. The trouble is you spend so much of your life second-guessing yourself that you don’t get a chance to live in the moment. Instead, you are caught in a constant fight-flight-or-freeze sympathetic loop.
I noticed a pattern in my practice that patients with autoimmune disease tend to be hard on themselves. I started looking into the research and I found this paper revealing that patients with autoimmune disease are more self-deprecating than controls, which confirmed my suspicions. Years of overwork and stress to prove your worthiness leads to chronic activation of your sympathetic system. Your stress activation system is closely linked with your immune system. The full mechanisms of action for self-criticism and immune activation are not fully worked out yet, but there is a connection.
Just like Dr. Brown said, perfectionism is a misguided tool to reduce or minimize the painful feelings of blame, judgement and shame. Criticizing yourself and striving for perfection unfortunately do not produce the desired outcome and can harm your health.
Instead, try holding a hand over your heart and saying to yourself: "I am enough."
LONELINESS
Another aspect to consider is loneliness. Loneliness actually changes how the immune system works. Cellular immunity is impaired, natural killer cells decline, and antibody titers rise. Loneliness triggers the fight/flight/freeze stress response. Humans have spent most of our existence as a species being supported and protected by each other. Loneliness signals to our body that we are in danger, which kicks up levels of inflammation and changes immune response.
The real kicker for me is that folks who have or develop a chronic illness, such as an autoimmune disease, have a higher risk for becoming socially isolated. So not only does loneliness increase the risk of developing an autoimmune disease, having an autoimmune disease increases your risk of becoming lonely.
We have so many mind-body medicine techniques at our disposal. Here are some resources I share with patients:
- Tara Brach has free downloadable talks and meditations on her website and is also available on your podcast app.
- Sharon Salzberg offers meditations for download at no cost on her website.
- John Makransky teaches a beautiful meditation style based on receiving love downloadable for free from his website.
- The Last Best Cure: My Quest to Awaken the Healing Parts of My Brain and Get Back My Body, My Joy, and My Life by Donna Jackson Nakazawa
- The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk
In all honesty it doesn’t matter what tools you pick as long as you actually do it. Don’t wait until it’s convenient, you have to incorporate relaxing activities into your daily routine. I find myself falling into the same trap I hear from patients - I can manage the tools on days that aren’t too busy but sometimes (read most of the time) I am ‘too busy’ to get in that exercise/meditation/coloring, etc. These are the days that you need it most. Creating new habits takes time and I hope that learning just how important stress management is for your health will help inspire you to take the time to cultivate new habits to build resilience.
If you are struggling with an autoimmune disease I recommend working with a naturopathic doctor to help identify the root cause and support your body. It is important to maintain all medications while working on your health from a holistic perspective. Autoimmune disease is serious and tissue destruction is permanent. Our goal with naturopathic treatment is to keep the medication dose stable and slow or stop the autoimmune destruction. I am often asked if patients can expect to stop their medication eventually and that depends on a variety of factors and is a decision made with the prescribing practitioner and patient.
References:
Self compassion as a predictor of interleukin-6 response to psychosocial stress
Compassion meditation reduced stress induced immune changes
Neural concomitants of immunity--focus on the vagus nerve
Personality traits and the immune system
IL-6 Induced by Social Stress
What is Mind Body Medicine






 RSS Feed
RSS Feed