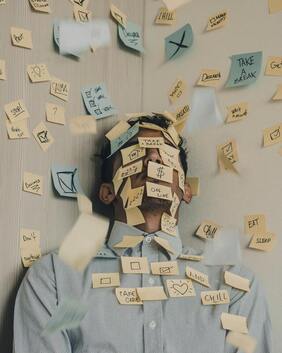
 Photo by Luis Villasmil on Unsplash
Photo by Luis Villasmil on Unsplash Is stress slowly killing you? It feels that way right now and surprisingly the answer might be yes! Lately I’ve been focusing my continuing education and reading on Psychoneuroimmunology defined by Merriam Webster as “a branch of medicine that deals with the influence of emotional states (such as stress) and nervous system activities on immune function especially in relation to the onset and progression of disease”. I had been noticing a significant relationship between mental/emotional stress and immune function since I started specializing in autoimmune disease but I had no idea there was an entire field of medicine devoted to this topic. I was reading an article and I noticed the author’s bio included psychoneuroimmunology and from then on I have been reading as much as I can about this fascinating topic.
Unfortunately the word ‘stress’ has become such a commonly used term and normalized in our society that when I try to broach this topic with patients I often hear, ‘I know stress is bad but let’s talk about XYZ diet and why I should follow it to fix my autoimmune disease’. Digging into the stress response is not a place many of us want to explore. I wonder if it’s because it feels too overwhelming and out of our control? Or maybe we just think that stress can’t possibly be the root cause of such significant illness? Why is it easier to blame food? Humans are poor reporters of their stress levels. It’s so indoctrinated in us that high levels of stress are normal that we no longer do a good job even recognizing that we are under high stress.
The work of Emily and Amelia Nagoski was helpful for me in breaking apart the stressors from the stress. Often we can’t control the stressors (work, kids, family) but we can control how we manage the stress in our body. Here are some clues that you might be struggling with stress (this is not a comprehensive list):
If you want to hear more about stressors vs stress and how to manage this check out the Nagoski sisters book- Burnout: The Secret to Unlocking the Stress Cycle. If you prefer to ‘cliff notes’ version check out this podcast episode interviewing the authors.
So how does this relate to our immune system? Well, our stress response system was designed to be activated in short bursts when we need to survive. Unfortunately, it’s activated much more often and we are feeling the consequences. When I talk to patients about stress many are familiar with the hormones adrenaline and cortisol. These two are our major players in the stress response but many other hormones are impacted when our stress response system is activated.
When we are under stress the following hormones are released:
When we are under stress the following hormones are suppressed:
We could deep dive into each of these hormones and how the changes impact you but this is a blog not a book. I will give you a few nuggets to get you thinking.
Cortisol suppresses our immune response, if you are under threat of bodily harm you don’t have time to waste resources fighting that pesky cold. The trouble is chronic infections are often lurking behind the scenes just waiting for your immune system to check out. EBV, varicella and herpes all contain stretches of DNA that sense glucocorticoid (cortisol) levels. When levels are higher these viruses reactivate. Isn’t that incredible (and also scary?)
Each of us process stress hormones differently for a variety of reasons. We are all biochemically unique and a great example of this is the COMT SNP. That’s quite the acronym huh? It stands for catechol-o-methyltransferase (COMT) single nucleotide polymorphism (SNP) and what it means is that there are some of us whose enzymes that process catechols a little differently. This can lead to higher levels of catechols such as adrenaline and noradrenaline staying in our system for longer. Folks with COMT mutations tend to have a bigger stress response to stressors than the average person.
Each of us processes stressors differently. As we grow up our brains learn how to appropriately respond to stress. When the young brain is constantly in a state of ‘fight or flight’ it causes lasting changes. The original research on how stressors in childhood impact long term health was called the ACE (Adverse Childhood Experiences) study. The results were profound. There is a direct association with the number of adverse events in childhood and risk of illnesses as an adult such as heart disease, IBS, diabetes, migraines, insomnia and more. This is after they controlled for diet, socioeconomic status, smoking, etc. Over 60% of us have experienced at least one significant adverse childhood experience.
In summary, chronic stressors lead to an overactive stress response that causes lasting damage. Each of us are unique in how we process these hormones and how easily we are triggered by stressful events. We are not great at recognizing and reporting how much stressors are causing an increase in the stress response. This is a really important piece in managing chronic illness.
Now that we understand how incredibly impactful our stress response is on our immune system what can we do about it?
Physical activity is probably one of the best tools that we have to combat the ever increasing levels of stress. Moving your body is a non-negotiable. We need 30 minutes of movement daily and this can be as simple as a walk outside.
Some other ideas for reducing the stress response include:
In all honesty it doesn’t matter what tools you pick for stress management as long as you actually do it. Don’t wait until it’s convenient, you have to incorporate relaxing activities into your daily routine. I find myself falling into the same trap I hear from patients- I can manage the tools on days that aren’t too busy but sometimes (read most of the time) I am ‘too busy’ to get in that exercise/meditation/coloring etc. These are the days that you need it most. Creating new habits takes time and I hope that learning just how important stress management is for your health will help inspire you to take the time to cultivate new habits to build stress resilience.
Unfortunately the word ‘stress’ has become such a commonly used term and normalized in our society that when I try to broach this topic with patients I often hear, ‘I know stress is bad but let’s talk about XYZ diet and why I should follow it to fix my autoimmune disease’. Digging into the stress response is not a place many of us want to explore. I wonder if it’s because it feels too overwhelming and out of our control? Or maybe we just think that stress can’t possibly be the root cause of such significant illness? Why is it easier to blame food? Humans are poor reporters of their stress levels. It’s so indoctrinated in us that high levels of stress are normal that we no longer do a good job even recognizing that we are under high stress.
The work of Emily and Amelia Nagoski was helpful for me in breaking apart the stressors from the stress. Often we can’t control the stressors (work, kids, family) but we can control how we manage the stress in our body. Here are some clues that you might be struggling with stress (this is not a comprehensive list):
- Depression/anxiety
- Anger, irritability
- Trouble sleeping or sleeping too much
- Problems with memory/concentration
- Feeling overwhelmed or unmotivated
- Digestive distress (constipation, diarrhea, bloating)
- Appetite changes
- Pain/tension in your head, chest, abdomen or muscles
- Lowered sex drive
- Irregular or painful menses
- Increase in blood pressure and/or heart rate
If you want to hear more about stressors vs stress and how to manage this check out the Nagoski sisters book- Burnout: The Secret to Unlocking the Stress Cycle. If you prefer to ‘cliff notes’ version check out this podcast episode interviewing the authors.
So how does this relate to our immune system? Well, our stress response system was designed to be activated in short bursts when we need to survive. Unfortunately, it’s activated much more often and we are feeling the consequences. When I talk to patients about stress many are familiar with the hormones adrenaline and cortisol. These two are our major players in the stress response but many other hormones are impacted when our stress response system is activated.
When we are under stress the following hormones are released:
- Glucagon (increase blood sugar)
- Prolactin (decrease reproduction)
- Endorphins and enkephalins (decrease pain)
- Cortisol (a major stress hormone)
When we are under stress the following hormones are suppressed:
- Estrogen
- Progesterone
- Testosterone
- Insulin
- Growth hormone
We could deep dive into each of these hormones and how the changes impact you but this is a blog not a book. I will give you a few nuggets to get you thinking.
Cortisol suppresses our immune response, if you are under threat of bodily harm you don’t have time to waste resources fighting that pesky cold. The trouble is chronic infections are often lurking behind the scenes just waiting for your immune system to check out. EBV, varicella and herpes all contain stretches of DNA that sense glucocorticoid (cortisol) levels. When levels are higher these viruses reactivate. Isn’t that incredible (and also scary?)
Each of us process stress hormones differently for a variety of reasons. We are all biochemically unique and a great example of this is the COMT SNP. That’s quite the acronym huh? It stands for catechol-o-methyltransferase (COMT) single nucleotide polymorphism (SNP) and what it means is that there are some of us whose enzymes that process catechols a little differently. This can lead to higher levels of catechols such as adrenaline and noradrenaline staying in our system for longer. Folks with COMT mutations tend to have a bigger stress response to stressors than the average person.
Each of us processes stressors differently. As we grow up our brains learn how to appropriately respond to stress. When the young brain is constantly in a state of ‘fight or flight’ it causes lasting changes. The original research on how stressors in childhood impact long term health was called the ACE (Adverse Childhood Experiences) study. The results were profound. There is a direct association with the number of adverse events in childhood and risk of illnesses as an adult such as heart disease, IBS, diabetes, migraines, insomnia and more. This is after they controlled for diet, socioeconomic status, smoking, etc. Over 60% of us have experienced at least one significant adverse childhood experience.
In summary, chronic stressors lead to an overactive stress response that causes lasting damage. Each of us are unique in how we process these hormones and how easily we are triggered by stressful events. We are not great at recognizing and reporting how much stressors are causing an increase in the stress response. This is a really important piece in managing chronic illness.
Now that we understand how incredibly impactful our stress response is on our immune system what can we do about it?
Physical activity is probably one of the best tools that we have to combat the ever increasing levels of stress. Moving your body is a non-negotiable. We need 30 minutes of movement daily and this can be as simple as a walk outside.
Some other ideas for reducing the stress response include:
- Singing
- Dancing
- Creative outlets
- Nurturing healthy relationships
- Breathwork
- Formal exercise
- Meditation/Mindfulness
- Spending time in nature
In all honesty it doesn’t matter what tools you pick for stress management as long as you actually do it. Don’t wait until it’s convenient, you have to incorporate relaxing activities into your daily routine. I find myself falling into the same trap I hear from patients- I can manage the tools on days that aren’t too busy but sometimes (read most of the time) I am ‘too busy’ to get in that exercise/meditation/coloring etc. These are the days that you need it most. Creating new habits takes time and I hope that learning just how important stress management is for your health will help inspire you to take the time to cultivate new habits to build stress resilience.


 RSS Feed
RSS Feed