Authored by Dr. Aidanne
Recovering from a COVID19 infection can be challenging enough, let alone living with long COVID symptoms after the infection clears. Digestive upset (ie. nausea, abdominal pain, vomiting) and bowel movement changes are among the more common long COVID symptoms. If you previously lived with a happy gut, this could significantly impact your new day to day life.
And why does it happen? How does the SARS-CoV2 virus affect gut and the microbiome.
To grasp this connection, we must first understand our biology. For those who may be new to this topic, the gut microbiome refers to the community of “flora” including bacteria, yeast, and viruses that colonize our intestines. They are meant to be there in a delicate balance and serve many beneficial purposes. They help us digest our foods, absorb nutrients, keep the intestinal lining healthy, fend off other invaders that may enter the system through our environment, lower inflammation, and make neurotransmitters such as serotonin that communicate with our brain.
This community keeps our bodies running smoothly but their balance is susceptible to damage from exposures in our environment such as infectious disease-causing organisms. We want a variety of beneficial species in the intestines with no one strain becoming dominant.
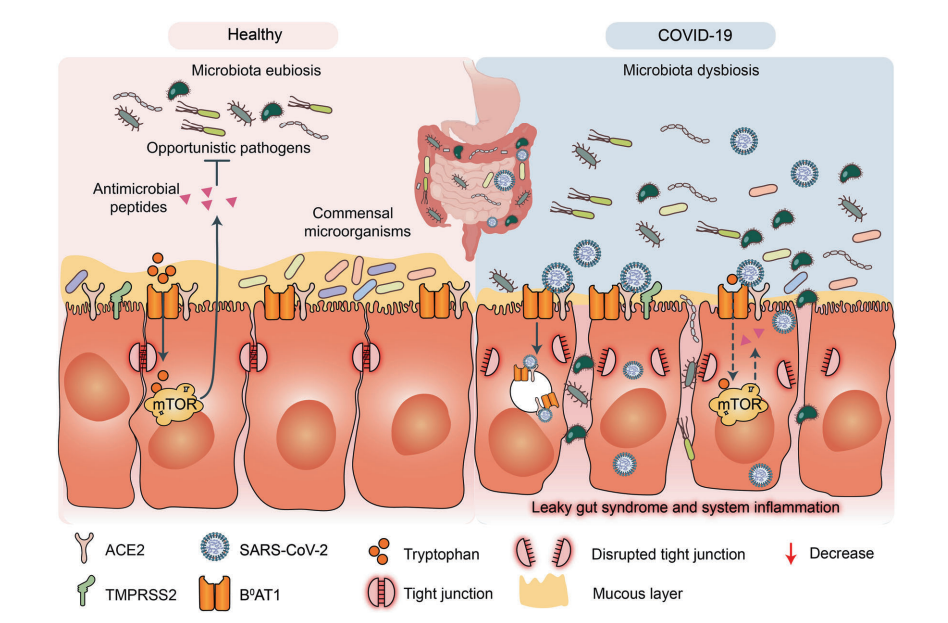
Various studies have shown that the stool samples of those who have contracted COVID-19 not only have a lower variety of beneficial microbes in their samples compared to a healthy counterpart but they also have a lower quantity of beneficial flora. If you think of the GI tract as a tube that only has so much space for microbes to fill, space that is left empty by the absence of beneficial flora will be filled with more problematic or opportunistic species (ie. Candida, Clostridium, Enterobacter, etc.).
Once these species seize the opportunity to establish themselves in the system, they wreak havoc by first inducing inflammation in the intestinal tissue. This inflammation then signals to the immune cells resting in the brush border of the intestine that we have something to fight off. To kill off these invaders, these local immune cells sound the alarm to their neighbors to make what are called cytokines. These are compounds that help guide the immune response but can further the inflammatory cycle if not kept in check.
Ultimately, the inflammation from this process wears down the protective mucus barrier to the brush border. It can also weaken the bonds called tight junctions that keep the cells of the GI tract close together, and weakened tight junctions contribute to intestinal hyperpermeability or “leaky gut”. If you think of a bucket with holes in it, you can expect that a lot of water will fall through. In a similar vein, if the intestinal lining is leaky we will not be able to digest our foods or absorb our nutrients well which can further contribute to imbalances in the local flora that are not prepared to pick up the leg work in feeding on undigested foods.
To cut this cycle and help the intestinal lining heal, naturopathic medicine offers a diverse set of tools including botanical medicines, probiotics, dietary counseling, and targeted nutritional supplementation.
Are you ready to start your journey? Let’s chat!
References:
And why does it happen? How does the SARS-CoV2 virus affect gut and the microbiome.
To grasp this connection, we must first understand our biology. For those who may be new to this topic, the gut microbiome refers to the community of “flora” including bacteria, yeast, and viruses that colonize our intestines. They are meant to be there in a delicate balance and serve many beneficial purposes. They help us digest our foods, absorb nutrients, keep the intestinal lining healthy, fend off other invaders that may enter the system through our environment, lower inflammation, and make neurotransmitters such as serotonin that communicate with our brain.
This community keeps our bodies running smoothly but their balance is susceptible to damage from exposures in our environment such as infectious disease-causing organisms. We want a variety of beneficial species in the intestines with no one strain becoming dominant.
Various studies have shown that the stool samples of those who have contracted COVID-19 not only have a lower variety of beneficial microbes in their samples compared to a healthy counterpart but they also have a lower quantity of beneficial flora. If you think of the GI tract as a tube that only has so much space for microbes to fill, space that is left empty by the absence of beneficial flora will be filled with more problematic or opportunistic species (ie. Candida, Clostridium, Enterobacter, etc.).
Once these species seize the opportunity to establish themselves in the system, they wreak havoc by first inducing inflammation in the intestinal tissue. This inflammation then signals to the immune cells resting in the brush border of the intestine that we have something to fight off. To kill off these invaders, these local immune cells sound the alarm to their neighbors to make what are called cytokines. These are compounds that help guide the immune response but can further the inflammatory cycle if not kept in check.
Ultimately, the inflammation from this process wears down the protective mucus barrier to the brush border. It can also weaken the bonds called tight junctions that keep the cells of the GI tract close together, and weakened tight junctions contribute to intestinal hyperpermeability or “leaky gut”. If you think of a bucket with holes in it, you can expect that a lot of water will fall through. In a similar vein, if the intestinal lining is leaky we will not be able to digest our foods or absorb our nutrients well which can further contribute to imbalances in the local flora that are not prepared to pick up the leg work in feeding on undigested foods.
To cut this cycle and help the intestinal lining heal, naturopathic medicine offers a diverse set of tools including botanical medicines, probiotics, dietary counseling, and targeted nutritional supplementation.
Are you ready to start your journey? Let’s chat!
References:
- Wang B, Zhang L, Wang Y, et al. Alterations in microbiota of patients with COVID-19: potential mechanisms and therapeutic interventions. Sig Transduct Target Ther. 2022;7(1):1-15.
- Bernard-Raichon L, Venzon M, Klein J, et al. Gut microbiome dysbiosis in antibiotic-treated COVID-19 patients is associated with microbial translocation and bacteremia. Nat Commun. 2022;13(1):5926.

 RSS Feed
RSS Feed