
What is Ferritin?
Ferritin is a protein found in almost all living organisms, from bacteria to humans. Its primary role is to store and release iron in a controlled manner, ensuring that cells have access to this essential mineral when needed. In humans, ferritin is primarily stored in the liver, spleen, and bone marrow, with smaller amounts circulating in the bloodstream.
The Iron Connection
Iron, often dubbed the "building block of life," is indispensable for various bodily functions, including oxygen transport, energy production, and DNA synthesis. However, iron is a double-edged sword. While crucial in the right amounts, excess iron can lead to oxidative stress and tissue damage.
Enter ferritin – the guardian of iron homeostasis. By encapsulating excess iron within its spherical shell, ferritin prevents the formation of harmful free radicals, safeguarding cells from oxidative harm. Moreover, ferritin acts as a reservoir, releasing iron when the body demands it, such as during periods of increased metabolic activity or blood loss.
Symptoms of Ferritin Imbalance
- Low Ferritin Levels (Iron Deficiency): Individuals with low ferritin levels may experience symptoms such as fatigue, pale skin, shortness of breath, weakness, and cognitive impairment. Iron deficiency anemia, characterized by insufficient iron stores, can significantly impact overall health and vitality.
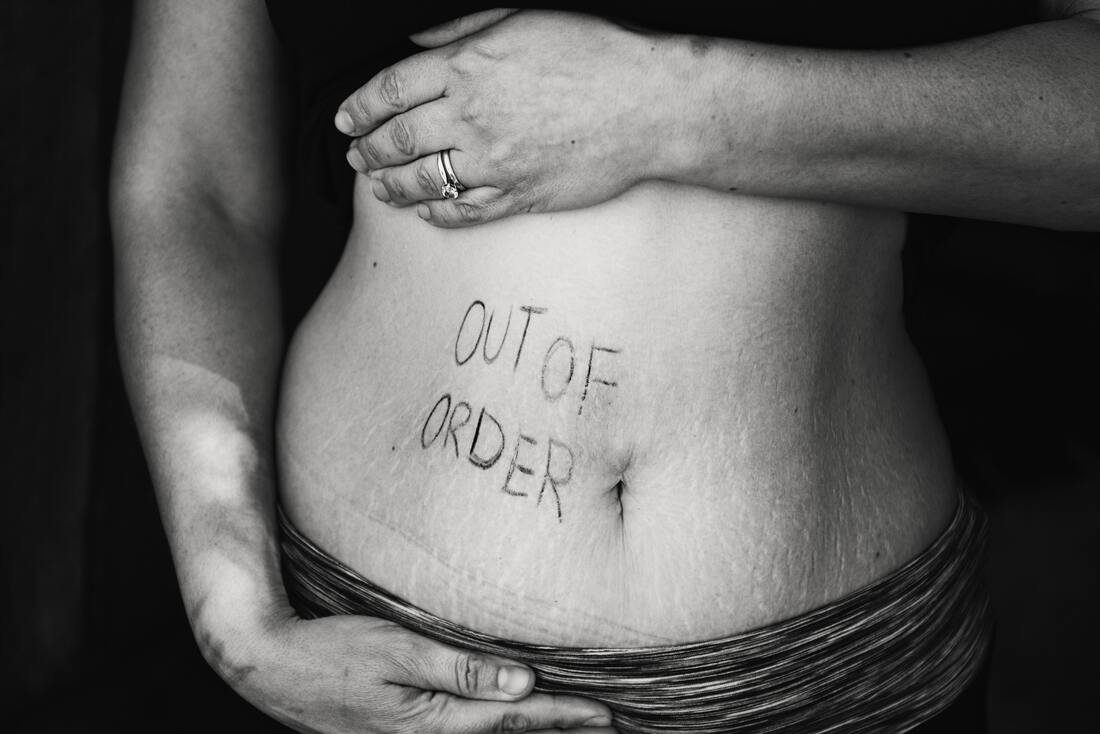
- High Ferritin Levels (Iron Overload or Inflammation): Conversely, elevated ferritin levels may indicate iron overload or inflammation. Symptoms of high ferritin levels can include joint pain, fatigue, abdominal discomfort, organ damage, and skin discoloration.
Testing Ferritin Levels
Assessing ferritin levels through blood tests provides valuable insights into iron status and overall health. Normal ferritin levels typically range from 12 to 300 nanograms per milliliter (ng/mL) for adults, with optimal levels falling within the mid range of this spectrum. Regular monitoring of ferritin levels can help identify deficiencies or excesses early on, allowing for prompt intervention and management.
Iron-Rich Diet and Supplementation
Maintaining adequate ferritin levels often involves consuming a balanced diet rich in iron-containing foods such as red meat, poultry, fish, beans, lentils, tofu, and dark leafy greens. Additionally, incorporating vitamin C-rich foods like citrus fruits, bell peppers, and strawberries can enhance iron absorption, thereby supporting ferritin production. In cases of documented iron deficiency, health care providers may recommend iron supplementation to restore ferritin levels. However, caution must be exercised with supplementation to avoid excessive iron intake, which can lead to adverse health effects.
The Intricacies of Ferritin and Thyroid Hormones
The synthesis of thyroid hormones is iron-dependent, meaning that iron plays a crucial role in the production of these hormones in the thyroid gland. Conversely, thyroid hormones can influence ferritin levels by regulating the expression of proteins involved in iron metabolism. Thyroid disorders, such as hypothyroidism and hyperthyroidism, can impact ferritin levels, highlighting the intricate interplay between these two systems and the importance of maintaining balance for optimal health.
Ferritin and Cognitive Function
Recent research has shed light on the association between ferritin levels and cognitive function, particularly in aging populations. A study investigating the impact of ferritin on various cognitive domains found that higher ferritin levels (>39) were significantly associated with better executive function and language skills in individuals aged 65 and older. This finding underscores the potential role of ferritin as a biomarker for cognitive health in aging populations. Furthermore, the study revealed that maintaining optimal ferritin levels may contribute to better cognitive performance in younger adults as well, highlighting the importance of ferritin in preserving cognitive function as individuals age.
Beyond Iron: Lesser-Known Connections of Ferritin
While ferritin's primary role is often associated with iron storage, emerging research has uncovered its involvement in various physiological processes beyond iron metabolism. Here are some lesser-known connections of ferritin to human health:
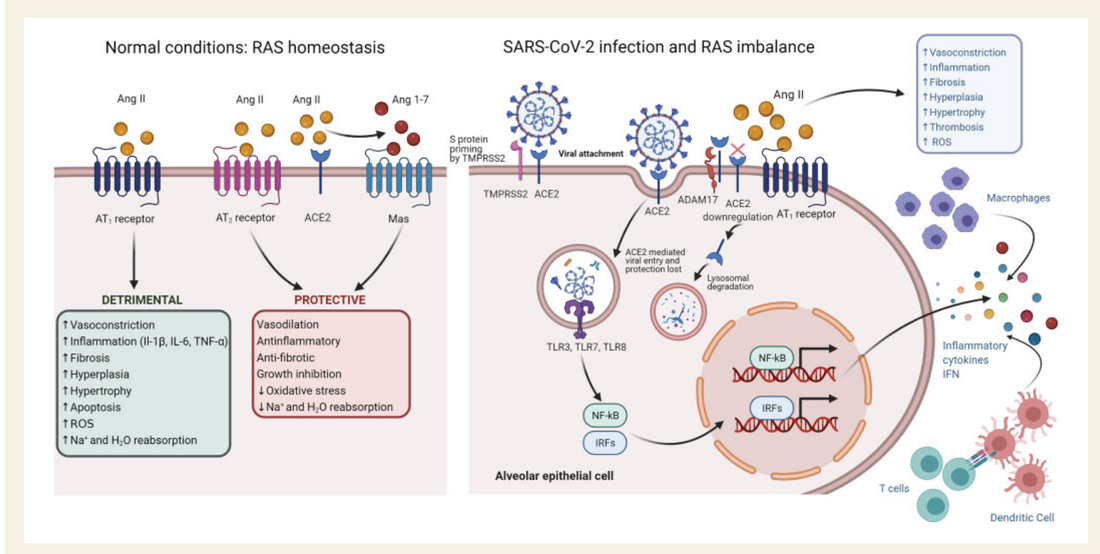
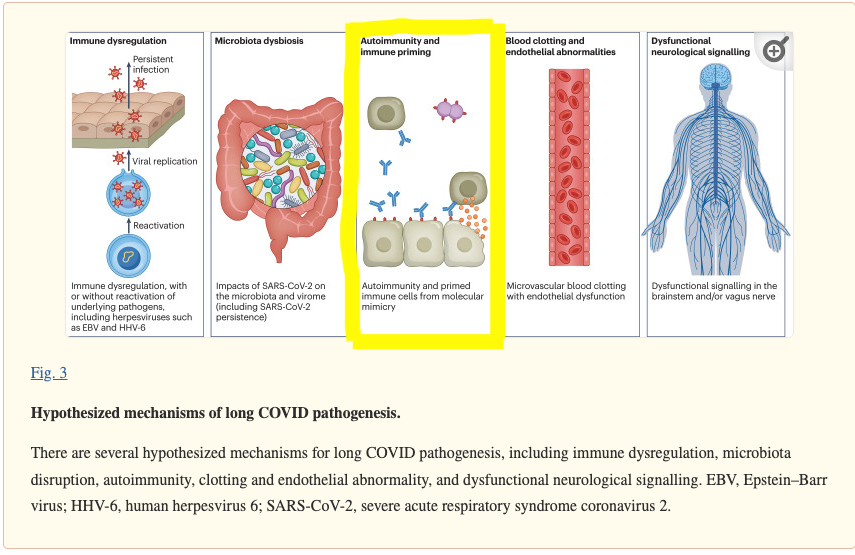
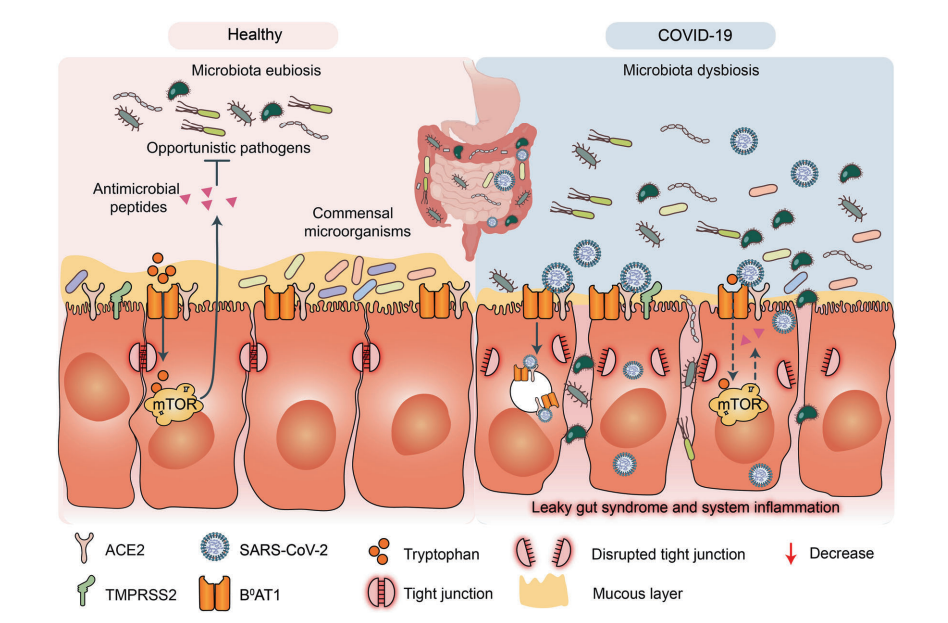
- Inflammation and Immune Response: Ferritin serves as more than just an iron storage protein; it also plays a role in the body's response to inflammation and immune activation. During times of inflammation, ferritin levels can rise significantly as part of the acute-phase response, helping to protect tissues from oxidative damage caused by inflammation.
- Neurological Disorders: Abnormal ferritin levels have been implicated in various neurological disorders, including Alzheimer's disease, Parkinson's disease, and multiple sclerosis. Iron dysregulation in the brain, often reflected by abnormal ferritin levels, has been linked to neurodegenerative processes and neuronal damage, highlighting the potential therapeutic implications of targeting ferritin in these conditions.
- Cardiovascular Health: Iron metabolism, including ferritin levels, has been associated with cardiovascular health. Both iron deficiency and iron overload can have adverse effects on the heart and blood vessels, emphasizing the importance of maintaining ferritin levels within a healthy range to support cardiovascular function.
- Metabolic Syndrome and Diabetes: Emerging evidence suggests a potential link between ferritin levels and metabolic syndrome, a cluster of conditions that increase the risk of heart disease, stroke, and type 2 diabetes. Elevated ferritin levels have been observed in individuals with metabolic syndrome, and some studies have suggested that ferritin may play a role in insulin resistance and glucose metabolism, though further research is needed to elucidate the precise mechanisms underlying this association.
- Cancer Risk and Progression: Aberrant ferritin levels have been implicated in various cancers, including breast cancer, liver cancer, and pancreatic cancer. High ferritin levels have been associated with increased cancer risk and poor prognosis in certain malignancies, highlighting the potential role of ferritin in cancer development and progression. It is hypothesized that iron, sequestered within ferritin, may promote tumor growth by fueling cancer cell proliferation and supporting angiogenesis, while inflammation-driven increases in ferritin levels may contribute to the pro-carcinogenic effects of the tumor microenvironment.
Caution with Iron Supplementation:
While iron supplementation may be necessary in cases of documented deficiency, excessive iron intake can lead to oxidative stress and adverse health effects. It is essential to seek healthcare guidance before initiating supplementation and to monitor ferritin levels regularly to ensure optimal iron status.
In conclusion, ferritin's significance extends far beyond its role as a simple iron storage protein, encompassing diverse aspects of human health and disease. Understanding the complexities of ferritin, from its basic functions to its broader implications, is crucial for promoting optimal health and well-being.
Fortunately, ferritin is a low cost biomarker tested. Consider talking with your provider about adding ferritin to your next blood screening tests.















 RSS Feed
RSS Feed