If you want more on this topic and you don’t want to continue reading check out this link to watch a Curiosity Corner where Jesse Haas and I discussed the documentary, "The Truth About Alcohol."
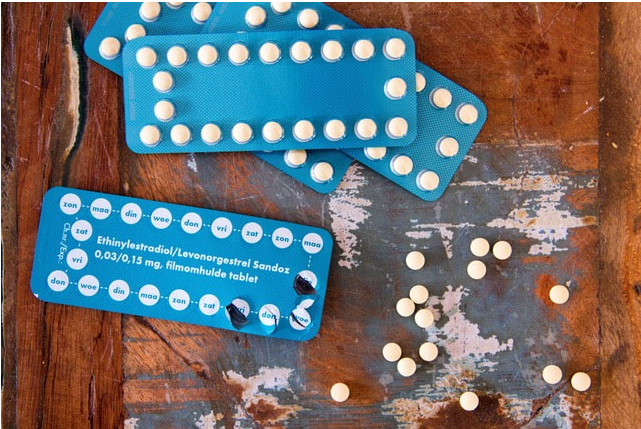
Alcohol use is so pervasive in our culture that it’s considered normal and safe. Unfortunately, alcohol is not a benign substance. In fact, it’s a known carcinogen. The UK spent 3.5 years reviewing all of the literature on alcohol and health and in 2016 overhauled its alcohol guidelines. The new guidelines are 14 units per week. To put that into context; a glass of red wine can be between 2-3 units depending on the strength of the wine and the size of the glass. For beer, a pint is typically between 1.5-2 units. So if you are drinking one or more alcoholic beverages per day you may be exceeding these guidelines. The UK also recommends 14 units or less regardless of your gender.
The main reason the UK took such a hard stance on alcohol was the research proving that alcohol is a potent carcinogen. Folks that regularly consume alcohol increase their risk of developing a wide range of cancers. Cancer is concerning but honestly, the cancer risk isn’t what really convinced me to reduce my consumption. How damaging alcohol is on our sleep is what did it for me. I don’t know about you but I have been so tired throughout the pandemic. The increase in daily stress and workload is a lot for us to carry. So when I started listening to Dr. Matthew Walker’s book, Why We Sleep, and learned about the relationship between alcohol and poor sleep I took action. Even 1 alcoholic beverage consumed hours before bed inhibits your ability to achieve REM sleep. Walker jokes that if you want to consume alcohol and still sleep well you have to start drinking with your morning coffee (please don’t try that). He goes on to discuss the shocking impact alcohol has on memory. I have heard from so many patients about memory trouble in the past year. Of course, the stress we are under will negatively impact memory but I wonder if alcohol consumption is playing a part for some folks as well.
You might be thinking, but a little red wine every day is good for me, right? Well, the only demographic that benefits from alcohol consumption are folks with ovaries who are 50+ years old and consume 2-3 glasses of wine per week. That’s it. So unless you fit in that demographic, the red wine you are drinking is likely not helping your heart. Alcohol contributes to leaky gut, depletes nutrients, and it weakens our immune system.
I know, I know I really shouldn’t be coming for your alcohol. It’s been a hard year. You feel that you need that wine or beer at night. I hear you. It’s been a very hard year. Most of us are exhausted and completely drained. It’s time to be honest, the alcohol is not helping.
What if you start with one day per week that you skip the alcohol and slowly increase to more days during the week? Can you find something truly nurturing to replace it with? An epsom salt bath? Hot tea? A stroll after dinner? A chat with a friend? Some people are better with abstention vs moderation. If that’s you then try a month without alcohol and see how your health changes. I know it's difficult but I think it's worth exploring the impact alcohol is having on your health and wellbeing.








 RSS Feed
RSS Feed